MPS IIIA is a severe and progressive disease that affects nearly all body systems1,2
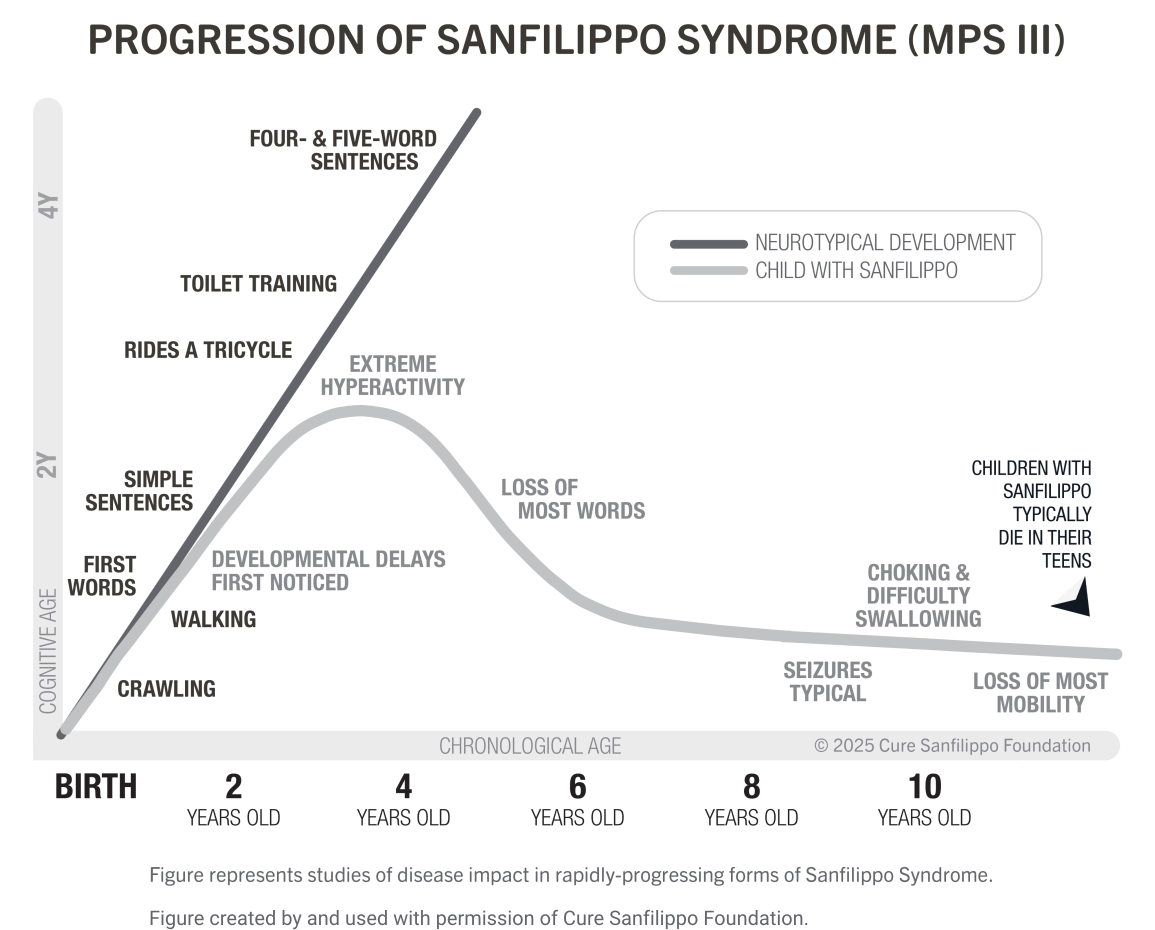
Children with MPS IIIA appear healthy at birth and develop normally until around 2 years of age when developmental delays and behavioral problems begin to emerge.1-5
Neurocognitive development plateaus as early as 3.5 to 4 years of age, after which children with MPS IIIA experience a decline in cognitive and motor skills.1,3,6 Eventually, children experience a decline in all motor functions, including speech, mobility, and swallowing.7,8 Premature death, often due to respiratory, neurologic, or gastrointestinal complications, typically occurs by 20 years of age.1,2,9
MPS IIIA can impact nearly all body systems
Although cognitive, neurologic, and behavioral issues are the hallmarks of MPS IIIA, nearly all body systems can be affected through the progressive course of the disease, with variability across individual children.1
Multisystemic manifestations of MPS IIIA20
- Vision problems
- Retinal damage
- Otitis media
- Hearing loss
- Recurrent sinusitis
- Tonsils and adenoid hypertrophy
- Tracheomalacia
- Sleep apnea
- Dysphagia
- Hepatosplenomegaly
- Diarrhea and/or constipation
- Umbilical and inguinal hernias
- Hydrocephalus
- Loss of language
- Mild valvular problems
- Reduced lung function
- Frequent coughs and colds
- Joint stiffness, pain, deformities or dislocation
- Scoliosis
- Early osteoporosis
- Clinodactyly
- Difficulty fully extending arms
- Knock knees
- Tight Achilles tendon
- Loss of mobility
Abbreviations: MPS, mucopolysaccharidosis; MPS IIIA, mucopolysaccharidosis type IIIA.
References
- Wagner VF, Northrup H. Mucopolysaccharidosis type III. 2019. In: Adam MP, Feldman J, Mirzaa GM, et al, eds. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024. Accessed January 2, 2025. https://www.ncbi.nlm.nih.gov/books/NBK546574/
- Lavery C, Hendriksz CJ, Jones SA. Mortality in patients with Sanfilippo syndrome. Orphanet J Rare Dis. 2017;12(1):168.
- Wijburg FA, Węgrzyn G, Burton BK, Tylki-Szymańska A. Mucopolysaccharidosis type III (Sanfilippo syndrome) and misdiagnosis of idiopathic developmental delay, attention deficit/hyperactivity disorder or autism spectrum disorder. Acta Paediatr. 2013;102(5):462-470.
- Fedele AO. Sanfilippo syndrome: causes, consequences, and treatments. Appl Clin Genet. 2015;8:269-281.
- Valstar MJ, Ruijter GJ, van Diggelen OP, Poorthuis BJ, Wijburg FA. Sanfilippo syndrome: a mini-review. J Inherit Metab Dis. 2008;31(2):240-252.
- Shapiro EG, Eisengart JB. The natural history of neurocognition in MPS disorders: a review. Mol Genet Metab. 2021;133(1):8-34.
- Shapiro EG, Nestrasil I, Delaney KA, et al. A prospective natural history study of mucopolysaccharidosis type IIIA. J Pediatr. 2016;170:278-287.
- Lanar S, Parker S, O’Neill C, et al. Understanding disease symptoms and impacts and producing qualitatively-derived severity stages for MPS IIIA: a mixed methods approach. Orphanet J Rare Dis. 2022;17:75.
- Thomas S, Ramaswami U, Cleary M, Yaqub M, Raebel EM. Gastrointestinal manifestations in mucopolysaccharidosis type III: review of death certificates and the literature. J Clin Med. 2021;10:4445.
- Cure Sanfilippo Syndrome. What is Sanfilippo syndrome. Accessed February 20, 2025. https://curesanfilippofoundation.org/what-is-sanfilippo/
- Shapiro E, Lourenço CM, Mungan NO, Muschol N, O’Neill C, Vijayaraghavan S. Analysis of the caregiver burden associated with Sanfilippo syndrome type B: panel recommendations based on qualitative and quantitative data. Orphanet J Rare Dis. 2019;14(1):168.
- Rumsey RK, Rudser K, Delaney K, Potegal M, Whitley CB, Shapiro E. Acquired autistic behaviors in children with mucopolysaccharidosis type IIIA. J Pediatr. 2014;164(5):1147-1151.
- Mahon LV, Lomax M, Grant S, Cross E, Hare DJ, et al. Assessment of sleep in children with mucopolysaccharidosis type III. PLoS One. 2014;9(2):e84128.
- Buhrman D, Thakkar K, Poe M, Escolar ML. Natural history of Sanfilippo syndrome type A. J Inherit Metab Dis. 2014;37(3):431-437.
- Kartal A. Delayed speech, hyperactivity, and coarse facies: does Sanfilippo syndrome come to mind? J Pediatr Neurosci. 2016;11:282-284.
- de Bode CJ, Dogterom EJ, Rozeboom AVJ, et al. Orofacial abnormalities in mucopolysaccharidosis and mucolipidosis type II and III: a systematic review. JIMD Rep. 2022;63(6):621-629.
- Baldini G, Fernando Palmejiani J, Bonevechio Sant’Anna JP, et al. Sanfilippo Syndrome: The Tale of a Challenging Diagnosis.J Inborn Err Metab Screen. 2020;8.
- Escolar M, Bradshaw J, Byers VT, et al. Development of a clinical algorithm for the early diagnosis of mucopolysaccharidosis III. J Inborn Err Metab Screen2020;8:e2020002.
- Galimberti C, Madeo A, Di Rocco M, Fiumara A. Mucopolysaccharidoses: early diagnostic signs in infants and children. Ital J Pediatr. 2018;44
- National MPS Society. A guide to understanding MPS III. Accessed February 6, 2025. https://mpssociety.org/wp-content/uploads/2023/05/MPS_III_Sanfilippo_Syndrome_Final.pdf